Guided Bone Regeneration (GBR) is a surgical procedure that promotes bone growth in deficient areas, enabling successful dental implant placement. It involves using barrier membranes and bone grafts to enhance osseointegration. Dental codes like D4266 and D4267 are essential for insurance reimbursement, ensuring accessibility for patients needing bone regeneration.
1.1 Definition and Purpose of GBR
Guided Bone Regeneration (GBR) is a dental surgical procedure that enhances bone growth in deficient areas to support dental implants. It uses barrier membranes and bone grafts to direct tissue regeneration, preventing unwanted cells from invading the defect. The purpose of GBR is to create sufficient bone volume and density for successful implant placement, addressing deficiencies caused by trauma, infection, or resorption. Dental codes like D4266 and D4267 are used to classify these procedures, ensuring proper documentation and insurance reimbursement.
1.2 Importance of GBR in Dental Implantology
Guided Bone Regeneration (GBR) is crucial in dental implantology for addressing bone deficiencies, ensuring implant stability, and achieving aesthetic outcomes. It enables successful implant placement in cases of insufficient bone volume due to trauma, infection, or resorption. GBR enhances osseointegration, improving long-term implant success rates. Dental codes like D4266 and D4267 are essential for documenting these procedures, facilitating insurance reimbursement and standardized care. GBR’s role in modern implantology underscores its significance in restoring oral function and patient confidence.

Dental Codes Related to Guided Bone Regeneration
Key dental codes for GBR include D4266, D4267, D7950, and D7953, essential for documenting bone regeneration procedures and ensuring proper billing and insurance reimbursement processes.
2.1 Overview of CDT Codes for GBR
CDT codes are essential for documenting guided bone regeneration procedures, ensuring accurate billing and insurance reimbursement. Key codes include D4266 for guided tissue regeneration, D4267 for regenerating supporting structures, and D7950/D7953 for bone replacement grafts in ridge preservation. These codes help standardize documentation, facilitating claims processing and ensuring proper compensation for GBR procedures. They are regularly updated to reflect advancements in dental techniques and materials, making them vital for modern dental practices.
2.2 D4266: Guided Tissue Regeneration
CDT code D4266 is specifically designated for guided tissue regeneration procedures. It applies to treatments addressing periodontal defects and bone loss, particularly in cases of moderate to advanced periodontitis. This code is essential for documenting procedures that involve the use of barrier membranes to regenerate lost tissue and bone around teeth. Proper use of D4266 ensures accurate billing and insurance reimbursement for GBR-related treatments, making it a critical component in dental coding for periodontal and bone regeneration therapies.
2.3 D4267: Regeneration of Supporting Structures
CDT code D4267 pertains to the regeneration of supporting structures, typically used when addressing advanced periodontal defects. This code is applied in cases requiring the regeneration of both bone and surrounding tissue to restore tooth support. It is essential for documenting procedures that focus on rebuilding the structural foundation around teeth, ensuring proper billing and insurance reimbursement for complex periodontal and bone regeneration treatments.
2.4 D7950: Bone Replacement Graft for Ridge Preservation
CDT code D7950 is designated for bone replacement graft procedures aimed at ridge preservation. This code is used when a bone graft is placed immediately after tooth extraction to maintain the alveolar ridge’s dimensions. It prevents bone loss, ensuring adequate support for future dental implants. D7950 is crucial for documenting ridge preservation procedures, facilitating accurate billing and insurance reimbursement for grafting techniques that safeguard bone integrity in preparation for implant placement.
2.5 D7953: Bone Replacement Graft for Ridge Preservation
CDT code D7953 is specifically designated for bone replacement grafts used in ridge preservation procedures. This code applies to grafting techniques that aim to maintain the alveolar ridge’s structural integrity, particularly after tooth extraction. D7953 is essential for documenting cases where bone grafting is performed to prevent bone resorption, ensuring a stable foundation for future dental implants. It plays a critical role in accurate billing and insurance reimbursement for procedures focused on preserving bone volume and shape.

Indications for Guided Bone Regeneration
Guided Bone Regeneration (GBR) is primarily indicated for addressing insufficient bone volume, periodontal defects, and ridge preservation after tooth extraction. It is essential for ensuring adequate bone support for dental implants, restoring lost bone structure, and preventing further bone resorption. GBR is particularly beneficial in cases where natural bone is insufficient to support implant placement, making it a critical procedure in modern dental implantology.
3.1 Insufficient Bone Volume for Dental Implants

Insufficient bone volume is a common indication for Guided Bone Regeneration (GBR), particularly when implant placement is compromised due to inadequate jawbone density or height. GBR addresses this by promoting new bone growth, ensuring sufficient support for dental implants. This procedure is crucial for patients with bone loss from periodontal disease, trauma, or resorption. By using barrier membranes and bone grafts, GBR helps restore the necessary bone structure, enabling successful implant placement and long-term stability.
3.2 Periodontal Defects and Bone Loss
Periodontal defects and bone loss often necessitate Guided Bone Regeneration (GBR) to restore lost tissue and prevent further deterioration. Advanced periodontitis can lead to significant bone degradation, compromising dental implant placement. GBR techniques, including membrane placement and bone grafting, help regenerate lost bone and tissue, addressing these defects. Dental codes like D4266 and D4267 are used to document these procedures, ensuring proper insurance reimbursement and patient access to essential treatments for periodontal-related bone loss.

3.3 Ridge Preservation After Tooth Extraction
Ridge preservation after tooth extraction is critical to maintain the alveolar ridge’s integrity, preventing bone loss and ensuring future implant placement. Guided Bone Regeneration (GBR) techniques, including bone grafts and membranes, are employed to preserve the socket and surrounding bone. Dental codes like D7950 and D7953 are used for bone replacement grafts, facilitating insurance reimbursement. This procedure is essential for maintaining the structural foundation for successful dental implants and restoring aesthetic and functional outcomes in patients with extracted teeth.
Materials and Techniques in GBR
GBR utilizes resorbable and non-resorbable membranes, bone grafting materials, and barrier coatings to enhance bone regeneration. These materials promote osteogenesis, ensuring optimal bone growth for dental implants.
4.1 Resorbable and Non-Resorbable Membranes
Resorbable membranes, made from materials like collagen or synthetic polymers, degrade naturally, eliminating the need for removal. Non-resorbable membranes, such as titanium or PTFE, are durable and often require surgical removal. Both types prevent soft tissue interference, allowing bone to regenerate effectively. Resorbable options reduce surgical steps, while non-resorbable membranes offer long-term stability. These materials are critical in guided bone regeneration, ensuring optimal bone growth for successful dental implant placement.
4.2 Bone Grafting Materials
Bone grafting materials are essential for guided bone regeneration, providing a scaffold for new bone growth. Common materials include autografts (patient’s own bone), allografts (donor bone), xenografts (animal-derived), and alloplasts (synthetic). Each material has unique properties, with autografts being the gold standard for osteogenic potential. Allografts and xenografts offer convenience, while alloplasts provide consistency. These materials are used to fill bone defects, promoting healing and supporting dental implant placement. Their selection depends on the patient’s needs and the defect’s complexity.
4.3 Barrier Coatings and Osteogenic Materials
Barrier coatings and osteogenic materials play a crucial role in guided bone regeneration by enhancing bone growth and preventing soft tissue invasion. These materials, such as osteogenic coatings and growth factors, are applied to membranes or grafts to stimulate cellular activity; Recent advancements include bioactive proteins and silk fibroin, which promote tissue regeneration. These innovations improve the efficacy of GBR procedures, ensuring better integration and long-term stability of dental implants.

Clinical Procedure and Steps
GBR involves pre-surgical planning, bone grafting, membrane placement, and post-surgical care. The procedure ensures proper healing and bone regeneration, typically requiring 4-6 months for optimal results.
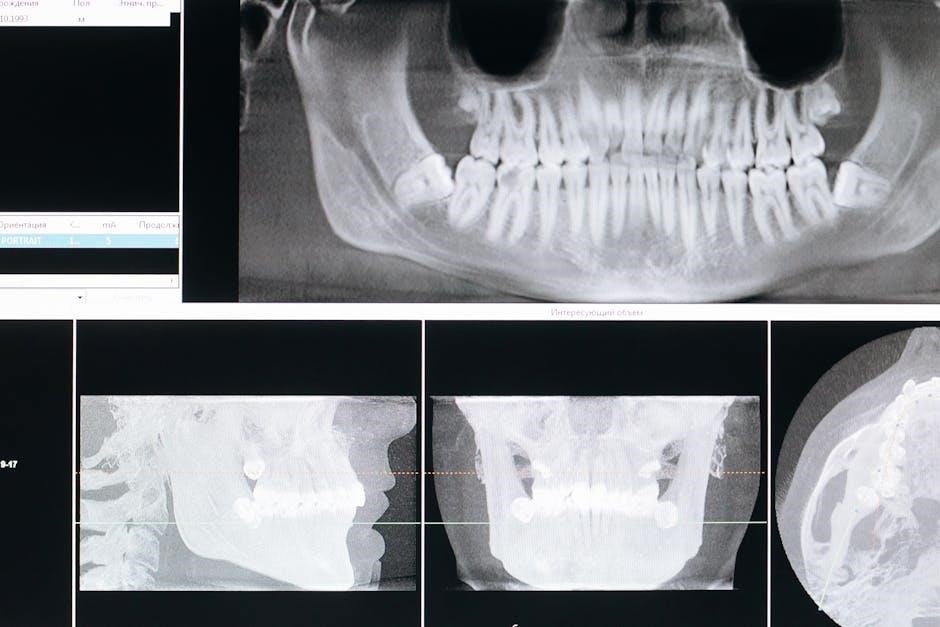
5.1 Pre-Surgical Evaluation and Planning
Pre-surgical evaluation involves assessing bone density and volume using CBCT scans and radiographs. Treatment planning includes identifying defect locations and determining the need for bone grafts or membranes. Dental codes like D7953 are considered for billing purposes. Patient-specific factors, such as medical history and implant placement goals, are evaluated to ensure personalized care. Accurate planning is crucial for successful GBR outcomes and minimizing complications during surgery.
5.2 Surgical Technique and Membrane Placement
The surgical technique involves creating an access flap to expose the bone defect. A resorbable or non-resorbable membrane is placed over the defect to prevent soft tissue invasion. Bone grafts are packed into the defect, and the membrane is secured. Dental codes like D4266 and D4267 are used for billing guided tissue regeneration procedures. Proper membrane placement ensures space maintenance for bone healing, promoting successful implant placement and long-term stability.
5.3 Post-Surgical Care and Follow-Up
Post-surgical care involves monitoring healing, managing pain, and preventing infection. Patients are advised to avoid strenuous activities, follow a soft diet, and maintain oral hygiene. Follow-up appointments are scheduled to assess bone regeneration and membrane integration. Dental codes like D4266 and D4267 are used for billing related procedures. Proper compliance with post-surgical instructions ensures optimal healing, supporting successful implant placement and long-term stability of the regenerated bone structure.
Market Trends and Research Advancements
The guided bone regeneration market is growing rapidly, with a projected CAGR of 4.6%, driven by innovations in membrane technology and long-term manufacturing partnerships like VIVOLTA.
6.1 Growth of the GBR Market
The guided bone regeneration market is experiencing significant growth, driven by increasing demand for dental implants and advancements in GBR techniques. In 2022, the market generated $727.7 million in revenue, with a projected CAGR of 4.6%. This growth is fueled by innovations in membrane technology and bone grafting materials, as well as rising awareness of periodontal disease treatments. Long-term manufacturing partnerships, such as VIVOLTA’s collaboration with Fibrothelium, are scaling production of advanced biomaterials, further boosting market expansion and accessibility for dental professionals.
6.2 Innovations in Membrane Technology
Recent advancements in membrane technology have revolutionized guided bone regeneration. Researchers have developed osteogenic barrier coatings that enhance bone growth and regeneration. Electrospun silk fibroin membranes, like those produced through partnerships such as VIVOLTA and Fibrothelium, offer improved biocompatibility and effectiveness. These innovations are critical for optimizing GBR procedures, ensuring better integration and long-term stability of regenerated bone. Such technological progress is driving the evolution of dental implantology and periodontal treatments, making GBR more predictable and successful for patients.
6.3 Long-Term Manufacturing Partnerships
Long-term manufacturing partnerships are crucial for advancing guided bone regeneration technologies. Companies like VIVOLTA and Fibrothelium collaborate to scale production of innovative materials, such as electrospun silk fibroin membranes. These partnerships ensure a stable supply of high-quality products, driving market growth and clinical adoption. By fostering such collaborations, manufacturers can optimize production processes, reduce costs, and deliver cutting-edge solutions for dental implantology and periodontal treatments, ultimately benefiting both clinicians and patients.

Success Rates and Clinical Outcomes
Guided bone regeneration (GBR) demonstrates high success rates, with stable bone formation and long-term implant survival. Patient satisfaction is elevated due to improved functional and aesthetic outcomes.
7.1 Efficacy of GBR in Implant Placement
Guided Bone Regeneration (GBR) significantly enhances dental implant placement success by addressing bone deficiencies. Studies show high efficacy, with over 90% success rates in achieving sufficient bone volume. The use of resorbable and non-resorbable membranes, combined with bone grafts, ensures proper healing and osseointegration. Dental codes like D4266 and D4267 facilitate insurance reimbursement, making GBR accessible for patients with periodontal defects or insufficient bone. This procedure is critical for achieving long-term implant stability and patient satisfaction.
7.2 Long-Term Stability of Regenerated Bone
Regenerated bone through GBR demonstrates excellent long-term stability, with studies showing maintained bone volume and density over years. The use of resorbable and non-resorbable membranes ensures proper healing and integration. Dental codes like D4266 and D4267 highlight the procedure’s recognition and reimbursement, ensuring patient access. Clinical outcomes reveal high success rates, with stable bone formation supporting dental implants long-term. This stability is crucial for both functional and aesthetic patient satisfaction, making GBR a reliable solution for bone deficiency cases.
7.3 Patient Satisfaction and Quality of Life
Patient satisfaction with GBR is high, as it restores functional chewing ability and aesthetic appeal. Successful bone regeneration enables stable implant placement, improving quality of life. Dental codes like D4266 and D4267 ensure proper documentation and reimbursement, making the procedure accessible. Patients often report enhanced confidence and comfort, highlighting the psychological benefits of GBR. Long-term outcomes show sustained satisfaction, with regenerated bone supporting implants effectively and maintaining oral health. This procedure significantly impacts patients’ overall well-being and dental functionality.
Cost Considerations and Insurance Coverage
GBR procedures vary in cost, depending on complexity and materials. Dental codes like D4266 and D4267 aid in insurance reimbursement, though coverage may differ. Patients should verify specifics with providers to understand out-of-pocket expenses and ensure proper billing for procedures.
8.1 Average Cost of GBR Procedures
The average cost of Guided Bone Regeneration (GBR) procedures varies widely, ranging from $1,000 to $5,000 or more per site, depending on the complexity of the case, materials used, and surgeon expertise. Factors such as bone grafts, membranes, and surgical time influence pricing. Dental codes like D4266 and D4267 are used for billing, but insurance coverage varies, often requiring pre-authorization. Patients should consult their providers and insurers to understand out-of-pocket expenses and ensure proper reimbursement for GBR treatments.

8.2 Insurance Reimbursement and Coding
Insurance reimbursement for GBR procedures depends on accurate coding and pre-authorization. Codes like D4266, D4267, D7950, and D7953 are used to bill for guided bone regeneration services. Coverage varies by insurer, with some policies reimbursing partial costs while others may deny claims if deemed non-essential. Patients should verify insurance eligibility and ensure proper documentation to maximize reimbursement. Dental teams must code procedures precisely to avoid claim denials and facilitate smooth processing.
8.4 Cost-Effectiveness of GBR
Guided Bone Regeneration (GBR) is a cost-effective solution for patients requiring bone augmentation before dental implants. While initial costs are high, GBR prevents more expensive complications and ensures long-term implant success. Procedures using codes like D4266 and D4267 are often reimbursed by insurance, reducing financial burden. Advanced materials, such as resorbable membranes, minimize recovery time and improve outcomes, making GBR a valuable investment for sustainable dental health and aesthetic results.
Guided Bone Regeneration is advancing rapidly, with a growing market and innovations in membrane technology. Future research focuses on enhancing materials and techniques for better outcomes.
9.1 Summary of GBR in Modern Dentistry
Guided Bone Regeneration (GBR) is a cornerstone in modern dentistry, addressing bone deficiencies to ensure successful implant placement. By using membranes and bone grafts, GBR enhances osseointegration and restores functional aesthetics. Dental codes like D4266 and D4267 facilitate insurance reimbursement, making these procedures accessible. The growing market and advancements in materials highlight GBR’s evolving role in improving patient outcomes and quality of life through innovative and effective bone regeneration techniques.
9.2 Future Directions in GBR Research
Future research in Guided Bone Regeneration (GBR) focuses on advancing membrane technology, such as electrospun silk fibroin, to improve bone regeneration efficiency. Innovations in osteogenic materials and barrier coatings are expected to enhance long-term stability. Partnerships like VIVOLTA and Fibrothelium aim to scale production of advanced biomaterials. These developments promise to optimize GBR outcomes, reduce healing times, and expand its applications in dental implantology, ensuring better patient care and aesthetic results.
Leave a Reply
You must be logged in to post a comment.